Presenting our 2021-2022 Powered by Pablove Research Recipients
During the pandemic when many foundations had to reduce or even slash their research budgets completely, we stayed strong. The Pablove Foundation and our Board of Directors believe so strongly in the research pillar of our mission that we doubled down on our investment, despite decreased donations due to COVID. Our kids need us to make safer cancer treatments a priority and we won’t let them down! Meet our newest research rockstars and learn more about their cutting-edge projects:


Delfim Duarte MD PhD, Instituto de Investigação e Inovação em Saúde da Universidade do Porto, Porto, Portugal
Studying: Acute Myeloid Leukemia
Project Title: Cell competition as a mechanism to eliminate minimal residual disease in acute myeloid leukemia
Acute myeloid leukemia (AML) accounts for about 20% of pediatric leukemias and is surpassing acute lymphoblastic leukemia (ALL) as the leading cause of death in children with leukemia. A major concern in a subgroup of AML patients is the persistence of minimal/measurable residual disease (MRD), which is composed by chemo-resistant leukemic cells and is associated with relapse. Dr. Duarte plans to use his Powered by Pablove research funding to develop and study a cutting edge approach to eliminating MRD in children being treated for AML.
The gist: Designing a cutting edge approach to cure children with high risk Acute Myeloid Leukemia

Amy Erbe-Gurel PhD, University of Wisconsin-Madison, Madison, Wisconsin
Studying: Neuroblastoma
Project Title: Improving Specific Targeting of Neuroblastoma Tumors through Bispecific SNIPER Antibody to Reduce Off-Target Toxicities
Neuroblastoma (NBL) is a type of childhood cancer afflicting roughly 800 children annually in the U.S. Patients with high-risk NBL are treated with a regimen that includes immunotherapy that binds to a marker that is present on both tumor cells and some nervous tissue. The binding of this immunotherapy to nervous tissue makes treatment extremely painful. Dr. Erbe-Gurel has developed a modified version of this immunotherapy that would target only tumor cells. With her Powered by Pablove research funding, she plans to study this modified treatment in live neuroblastoma models.
The gist: Improving care for children with neuroblastoma by curing their disease with less painful side-effects.
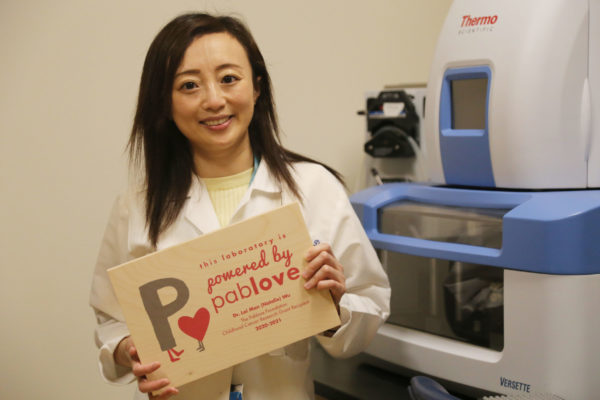
Lai Man (Natalie) Wu PhD, Children’s Hospital Medical Center, Cincinnati, OH
Studying: Malignant Peripheral Nerve Sheath Tumor (MPNST)
(RENEWAL) Project Title: Identification of cellular diversity and tumor-initiating cells driving NF-to-MPNST and drug resistance by single-cell multiomics for targeted therapy
Supported in part by Hanna’s Hoops 4 Healing
Neurofibromatosis type I (NF1), an inherited condition in children, affects one in every 3,000 individuals worldwide. Although benign in nature, in some cases, the slowly growing NF1-mutated nerve tumors can become malignant peripheral nerve sheath tumors (MPNST), killing 50% of the patients within five years. With 1 year of Powered by Pablove funding under her belt, Dr. Wu has begun to unravel the puzzle of how benign neurofibromas (NF) become cancerous MPNST. With a second year of funding, she plans to continue mapping out the transformation of cells from benign to malignant. Further, Dr. Wu will target points on that pathway with already established drugs that she believes can inhibit these cells from becoming cancerous.
The gist: Examining how a benign condition can lead to Malignant Peripheral Nerve Sheath Tumors and testing potential therapies

Thais Armangue MD PhD, Institute for Biomedical Research August Pi i Sunyer, Barcelona, Spain
Studying: OMS
(RENEWAL) Project Title: Opsoclonus myoclonus syndrome: a novel approach to antigen identification and disease modeling
Grant funded in partnership with The Viswanatha Family + Friends.
All the way in Barcelona, Spain, Dr. Armangue is studying a rare autoimmune condition called Opsoclonus-myoclonus Syndrome (OMS). During her first year of Powered by Pablove funding, Dr. Armangue used a novel technical approach to successfully identify a new antibody in a subgroup of OMS patients and demonstrate its importance for brain cell function. With an additional year of funding, Dr. Armangue and her team plan to expand on these successes with further antibody studies. In addition, they plan to explore the role of another part of the immune system, T-cells, in causing OMS.
The gist: Using novel techniques to understand the development of Opsoclonus-myoclonus Syndrome
Learn more about our research grants and what we’ve funded at: pablove.org/grants
